Reconstructive Urology
Male reconstructive urology (also called male genitourinary reconstruction) can be used to treat physical abnormalities, repair trauma related to major surgery or accidents, or manage certain bladder control problems like incontinence and overactive bladder.
Reasons for Reconstructive Procedures
Your doctor may have a number of reasons for having to perform male reconstructive urological techniques to correct complications due to disease, injury or major medical procedures.
Urethral Strictures
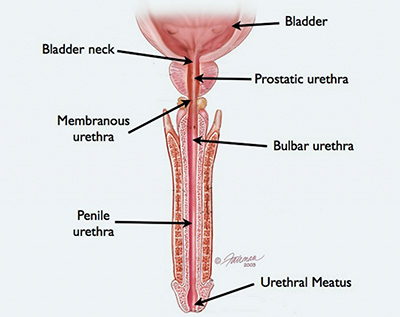
Narrow areas in the urethra that can obstruct urine flow are called urethral strictures. Men are rarely born with urethral strictures, which develop over time due to infection or medical procedures involving the urethra. They may be caused by inflammation or scar tissue from surgery, urinary tract infections, injury or repeated catheterization.
Other risks of developing urethral strictures include:
- sexually transmitted infection (STI)
- procedures that place a tube into the urethra, such as a catheter or cystoscope
- benign prostatic hyperplasia (BPH)
- injury to the pelvic area
- repeated swelling and inflammation of the urethra, called urethritis
Treatment for urethral strictures can include non-surgical urethral dilation but where surgery is necessary, an open urethroplasty is generally performed and the urethra reconstructed. Another option is endoscopic procedure called optical urethrotomy, where the urethra is incised to widen the lumen. There are currently no medications to treat urethral strictures.
External Trauma
Trauma to the urethra, prostate and bladder are often the result of major injuries to the pelvis or from blunt-force trauma and can require surgery to repair damage, realign the urinary tract or remove scar tissue post-care. Common injuries include damage to the bladder, tears or severe inflammation of the prostate or blockages of the urethra.
Incontinence
Surgery can be used to treat cases of overflow incontinence and stress incontinence by either reshaping the urethra, supporting the urethra or adding nerve stimulation to assist with bladder control. Surgery to correct incontinence following a prostatectomy is common.
Reconstructive Procedures
Artificial Urinary Sphincters (AUS)
Artificial urinary sphincters (AUS) are used to treat stress incontinence, where significant urinary leakage occurs during exercise, coughing, sneezing, laughing, lifting heavy objects, or other body movements. Your urinary sphincter normally prevents urinary flow through compression and pressure transmission, but when the sphincter weakens or is damaged, an artificial urinary sphincter can be inserted to mimic the biological urinary sphincter.
An artificial urinary sphincter has three parts:
- An inflatable cuff that fits around your urethra that, when inflated, closes off your urethra to stop the flow of urine or urinary leakage.
- A balloon implanted under your belly muscles.
- A pump inserted into your scrotum that includes a pump which can control the cuff.
Once the AUS is in place, you can use the pump to deflate the cuff, opening your urethra to allow you to urinate. The cuff will automatically re-inflate on its own in 90 seconds, closing the urethra and preventing urinary leakage from stress incontinence.
Urethral Reconstructive Surgery
Urethroplasty
Open urethral reconstruction called urethroplasty is the most common treatment for urethral strictures. Urethroplasty can be performed by two basic methods: The first is excision and anasmotomis (primary repair), which involves complete removal of the narrowed part of the urethra and the rejoining of the segments to form a new urethra. The second method involves grafted tissue used to enlarge the narrowed segment of the urethra, creating a wider passage for urine flow.
Mitrofanoff Procedure
A Mitrofanoff appendicovesicostomy, also known as the Mitrofanoff procedure, uses the appendix to create a passageway between the urinary bladder and the skin’s surface. The procedure is usually performed for patients who require constant catheterizations (like paraplegics or those with spina bifida) or when the urethra is severely blocked.
The Mitrofanoff procedure uses the appendix to create a new natural passageway from the bladder to the surface of the skin. One end of the appendix is connected to the bladder and the other to the surface of the skin to form an organic passage called a Mitrofanoff canal. A catheter is threaded through the new passageway into the bladder where urine is drained several times a day.
Ileal Conduit Formation
The simplest and most common method of diverting urine from the bladder is an ileal conduit (ileal refers to a section of the small intestine). People suffering from bladder conditions like nerve damage or bladder cancer often undergo ileal conduit formation surgery. An ileal conduit is formed using part of the small bowel to create and organic conduit from the bladder to the surface of the skin and out of an opening called a stoma. Urine flows from the bladder through the ileal conduit and into a watertight pouch placed over the stoma. The pouch will continually fill with urine and can be emptied at any time.
Ileal Neobladder
If the urethra is functioning correctly, other forms of urinary diversion can be utilized, such as an ileal neobladder. In an ileal neobladder procedure, the small bowel is used to make a new bladder (“neo” meaning “new”) which is joined back to the urethra. No external collection devices are needed, and patients can continue to use the toilet normally.
Indiana Pouch
Similar to the ileal neobladder, an Indiana pouch takes a section of the small bowel and a section of the large bowel to construct a reservoir pouch for urine. The Indiana pouch also constructs an organic passageway out of the body using the small bowel as a valve. The large bowel pouch acts like a bladder and stores the urine, while the end of the small bowel is brought out onto the surface of the skin, usually in or around the umbilicus area. This opening, known as a flush stoma, is used to pass a catheter and drain the pouch.
Ureteral Reimplantation
Ureteral reimplantation surgery is used to treat reflux, a condition in which urine from the bladder flows back up into the kidneys through tubes that connect them to each other. This is primarily done in the pediatric population, although performed less commonly in adults for specific reasons. Ureteral reimplantation rearranges the tubes to stop urine from backing up into the kidneys, which can cause scarring and permanent damage.
Pediatric Reconstructive Surgery
Hypospadias Repair
Hypospadias repair surgery is used to correct one of the most common birth defects in boys. Hypospadias occurs when the urethra doesn’t end at the tip of the penis but instead on the underside, middle or bottom of the penis, or in more severe cases in or behind the scrotum. Surgery is most often done when boys are between 6 months and 2 years old. Surgery is done as an outpatient and the child rarely has to spend a night in the hospital.
Sexual Dysfunction Surgery
Erectile Dysfunction
Erectile dysfunction (ED) is characterized by the inability to develop or maintain an erection during sexual intercourse. Smoking, Diabetes, atherosclerotic heart disease, aging and trauma from prostatectomy surgery are all leading causes of ED and can be treated with penile prostheses surgery. Nonsurgical treatments are usually exhausted before prostheses surgery is advised, but the surgery is reliable with a satisfaction rate of nearly 100 percent.
The prosthesis can be semi-rigid, malleable rod implant or an inflatable implant. A semi-rigid, malleable rod implant implants two matching cylinders into the penis. To achieve an erection, you manually adjust the position of the penis, providing rigidity. Surgery is relatively simple and there’s a high success rate, but it does replace the ability to achieve a normal erection. Inflatable implant surgery also implants two cylinders into the penis but with a pump placed in the scrotum and a reservoir placed beneath the tissue of the abdomen. To achieve erection, you squeeze the pump, which moves fluid up from the reservoir into the cylinders in the penis. The success rate for this surgery is also high, but inflatable implants need to be replaced every seven to 10 years.
Surgery to repair Peyronie’s Disease
Peyronie's disease is characterized by the development of a lump on the shaft of the penis that is usually the result of an acute or chronic injury during sexual relations. This lump is scar tissue that forms on the lining of the erectile body which, in some cases, however, can become progressively harder, causing the penis to curve during erection. The scar can result in curvature that makes it difficult to impossible to have sexual intercourse. If you develop a lump or what feels like scar tissue anywhere on the penis, it is important to seek consultation from a Beaumont urologist.
The incidence of Peyronie's disease is estimated to be between 1 to 3 percent, though the condition is likely to be under-reported. Peyronie’s disease occurs most often in middle-aged men but can occur in men from 20 to 70 years of age.
Peyronie's disease may shrink or disappear without treatment, so medical experts suggest waiting a full year before contemplating surgery. There are three primary types of procedures used to address Peyronie's disease:
- Penile Plication Procedures: These procedures involve a tuck procedure on the side opposite to the scar, shortening the long side of the penis. This procedure is simple and preserves preoperative erection ability but can include loss of penile length.
- Penile Prosthesis Surgery: Placement of a penile implant allows immediate correction of the penile curvature as well as allowing fully rigid erections. This procedure is generally reserved for men with combined erectile dysfunction and penile curvature.
Plaque Incision/Excision and Grafting: These procedures involve the complete or partial removal of the plaque or its incision, with the placement of a graft into the space left by the technique. This approach is typically not associated with loss of penile length but men can develop postoperative erectile dysfunction and prolonged loss of penile sensation.
